- What Is Birth Control and What Can It Be Used For?
- What Is the “Right Age” to Start Birth Control?
- What Birth Control Methods Are Most Appropriate for Teen Girls?
- What are the Risks And/Or Long-Term Effects of Birth Control?
Navigating the topic of birth control with your teenager can be challenging, and it’s common for parents to feel unsure about when to start these conversations. Just know that by the age of 18, more than half of all teenagers have engaged in sexual activity.
Although teen pregnancy rates have decreased in the United States, there are still over 200,000 infants born to teenage mothers each year. According to research from the CDC, 90% of sexually active teens use some form of birth control, with pills and condoms being the most popular choices.
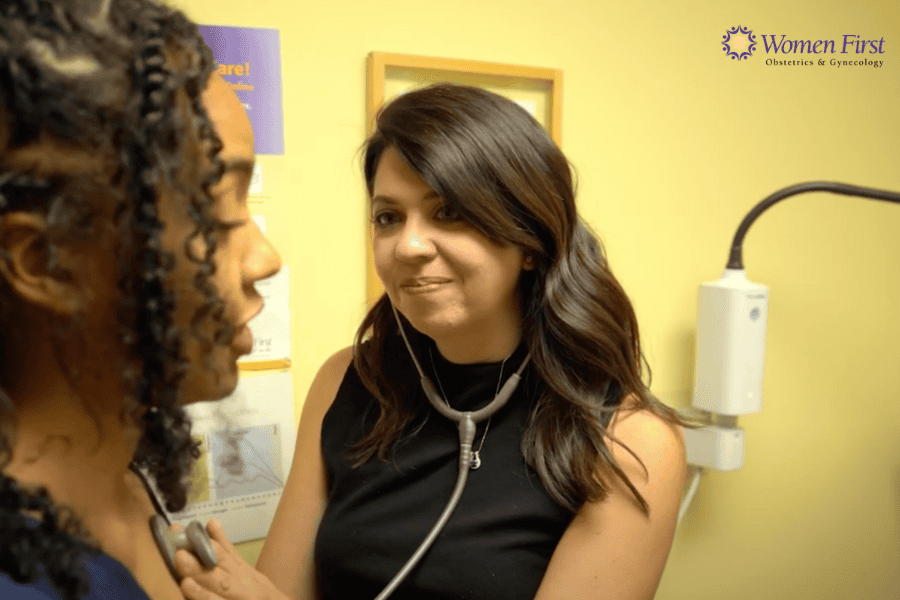
As parents, we recognize the significance of having informed discussions about reproductive health and when to initiate birth control. In this article, we will explore how to approach this subject with the guidance of Katherine Shannon, M.D., a board-certified obstetrician and gynecologist at Women First. We will also provide additional information on when to start birth control to help you make informed decisions and support your teenager’s reproductive health.
What Is Birth Control and How Its Used Today
 Contraception, also known as birth control, is the use of medication, devices, or surgical procedures to prevent pregnancy. It includes various types, ranging from reversible to permanent methods. Additionally, certain forms of contraception can also safeguard against sexually transmitted diseases (STDs).
Contraception, also known as birth control, is the use of medication, devices, or surgical procedures to prevent pregnancy. It includes various types, ranging from reversible to permanent methods. Additionally, certain forms of contraception can also safeguard against sexually transmitted diseases (STDs).
Dr. Shannon emphasizes the importance of considering the broader usefulness of today’s birth control.
“Birth control is not only for sexually active individuals, but it can also be beneficial for anyone experiencing heavy periods, period pain, or other symptoms.”
What Is the “Right Age” to Start Birth Control?
 The right age depends on the daughter’s comfort and the parent’s consent. However, it’s best to include an OB/GYN after talking to your teen about it.
The right age depends on the daughter’s comfort and the parent’s consent. However, it’s best to include an OB/GYN after talking to your teen about it.
Dr. Shannon recommends, “If there are no issues, I advise seeing your doctor before becoming sexually active or by the age of 21, whichever comes first.”
Typically, age 16 emerges as the most prevalent time for initiating birth control, allowing young women to establish their menstrual cycles before potentially disrupting them.
“Any menstruating person is welcome to come for an appointment to discuss how we might make that part of their lives easier,” says Dr. Shannon.
In addition to its primary function of preventing unwanted pregnancies, hormonal birth control aids in regulating periods, reducing ovulation, and potentially diminishing the risk of certain types of ovarian cancer.
Nevertheless, the decision to begin birth control is deeply personal and warrants careful discussion among parents, healthcare providers, and the young woman herself. While some girls may feel prepared at a younger age, others may not have reached the necessary psychological or emotional maturity level to manage the medical regimen effectively.
This is why talking to a doctor is so important that all questions and concerns are addressed so you can make the best decision.
What Birth Control Methods are Most Appropriate for Teen Girls?
The birth control pill remains the most commonly prescribed method for teenage girls. However, many mothers express concerns about their daughters’ ability to adhere to the pill’s daily regimen. Forgetting to take the pill can lead to more frequent bleeding and increase the risk of an unintended pregnancy.
For teens who struggle with forgetfulness, alternative options may be more suitable: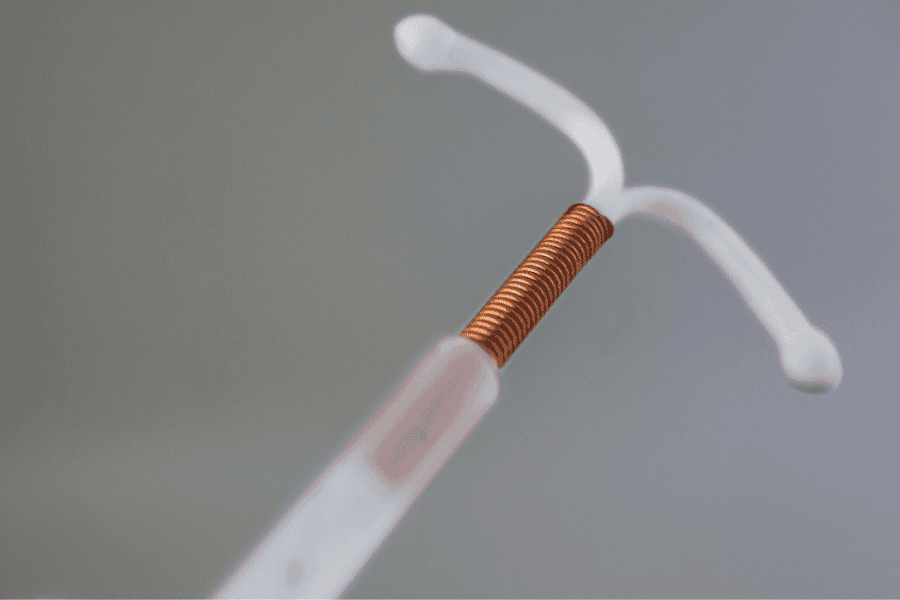
- Intrauterine Device (IUD): IUDs are a type of long-acting reversible contraception (LARC) that offers over 99% protection against pregnancy. There are two main types: progestin-containing IUDs (such as Skyla and Mirena), which last 3 to 5 years, and copper IUDs (Paragard), which last about ten years. While the copper IUD doesn’t contain hormones, it interferes with sperm movement and egg fertilization.
- Implant: The progestin insert, Nexplanon, is a small rod inserted under the skin that provides over 99% protection against pregnancy for up to 3 years.
- Injection: Depo-Provera is an injectable birth control given four times a year.
- Vaginal Ring: The NuvaRing is a flexible ring that releases hormones to prevent ovulation. It’s left in place for three weeks and removed for the fourth week. This option offers similar effectiveness to the birth control pill.
It’s important to note that while hormonal birth control methods are effective against pregnancy, they do not protect against sexually transmitted diseases. Therefore, it’s essential to emphasize the use of condoms alongside any hormonal birth control method to prevent STD transmission.
What are the Risks And/Or Long-Term Effects of Birth Control?
Many contraceptive methods share similar side effects, although they differ in certain aspects:
Injection (Depo-Provera)
Prolonged use of the birth control shot, Depo-Provera, has been associated with a potentially irreversible loss of calcium from the bones, according to recent studies. Patients are advised not to use Depo-Provera for more than five years. This information is particularly pertinent for teenagers and their parents considering birth control options, as starting Depo-Provera earlier may require switching methods as the teen reaches young adulthood.
Long-Acting Reversible Contraceptives (LARC) or IUDs
IUDs that contain progestin often cause irregular bleeding for the first three to six months while the body gets used to the hormone. This is the same side effect that women experience when they take the birth control pill. While this bleeding is typically not severe, it may persist or be bothersome. Some users may experience amenorrhea. Rarely, complaints include bloating, weight gain, headaches, or acne.
- The copper IUD does not regulate menstrual periods as it does not contain hormones. Consequently, a slightly heavier period is the most common side effect.
- Rarely, an IUD may dislocate outside the uterine cavity, moving into the uterine muscle or pelvic cavity. However, complete expulsion is rare, occurring in only 2-10% of cases.
- Insert: Patients who opt for an insert may experience adverse changes in their bleeding patterns or similar side effects to those observed with progestin-containing IUDs (such as headache, bloating or weight gain, acne, or depression).
Although most methods are generally safe, some may cause side effects such as irregular bleeding, abdominal discomfort, or mood changes.
Next Steps for Starting Birth Control for the First Time
When it comes to deciding on birth control, Women First of Louisville is always here to support you at every step. Our team is committed to providing personalized care and addressing all your reproductive health concerns.
Whether you need guidance on birth control options or want to schedule an appointment, we are here to help. Don’t hesitate to schedule an appointment with any of our doctors today. Your health is our top priority.
