 Gynecological cancers, including uterine, ovarian, and cervical cancers, often have subtle symptoms that can be easily overlooked. Recognizing these early indicators leads to a timely diagnosis and treatment.
Gynecological cancers, including uterine, ovarian, and cervical cancers, often have subtle symptoms that can be easily overlooked. Recognizing these early indicators leads to a timely diagnosis and treatment.
September is Gynecological Cancer Awareness Month, a time to raise awareness about cancers that affect women’s reproductive system. This month-long observance aims to educate the public about the importance of early detection, the latest advancements in treatment, and the critical need for regular screenings.
At Women First, we provide exams, screenings, and education to help women understand their symptoms and whether they’re experiencing warning signs of cancer. Read on to learn about the most common gynecological cancers, warning signs to watch for, and differentiating between common discomforts and potential red flags.
Understanding Gynecological Cancers
Gynecological cancers refer to cancers that originate in a woman’s reproductive organs. The most common types are uterine, ovarian, and cervical cancer. Early detection is essential as it significantly improves the chances of successful treatment and survival.
Common Symptoms of Uterine Cancer
- Abnormal Uterine Bleeding
- Bleeding that is irregular or heavy
- Postmenopausal Bleeding
- Bleeding or spotting that occurs after menopause
- Pelvic Pain
- An enlarged uterus can cause pelvic pain
Common Symptoms of Ovarian Cancer
 Abdominal Bloating
Abdominal Bloating- Persistent bloating that doesn’t go away and feels different from typical premenstrual or post-meal bloating.
- Pelvic or Abdominal Pain
- Unexplained and consistent pain in the lower abdomen or pelvic region.
- Difficulty Eating or Feeling Full Quickly
- A noticeable appetite or feeling full decreases after eating only a small amount.
- Frequent Urination
- A sudden increase in the frequency of urination.
- Changes in Bowel Habits
- New and persistent constipation or diarrhea.
Common Symptoms of Cervical Cancer
- Unusual Vaginal Bleeding
- Bleeding between periods, after intercourse, or post-menopause that is not part of your regular menstrual cycle.
- Abnormal Vaginal Discharge
- Discharge that is watery, bloody, or has a foul odor.
- Pelvic Pain
- Pain during intercourse or at other times that is persistent and unexplained.
- Painful Urination
- Discomfort or pain when urinating that is not associated with a urinary tract infection.
- Lower Back Pain
- Persistent lower back pain that is not related to physical activity or injury.
Risk Factors to Consider
Understanding the risk factors helps in assessing the likelihood of developing these cancers:
 Age: Women over 50 are at higher risk for uterine and ovarian cancer.
Age: Women over 50 are at higher risk for uterine and ovarian cancer.- Family History: A family history of ovarian or uterine cancer increases risk.
- PCOS or Anovulation: not ovulation regularly increases uterine cancer risk because there is a lack of progesterone
- HPV Infection: Persistent infection with high-risk types of human papillomavirus (HPV) is the primary cause of cervical cancer.
- Genetic Mutations: BRCA1 and BRCA2 gene mutations significantly increase the risk of ovarian cancer. Lynch Syndrome increases the risk of uterine cancer.
- Lifestyle Factors: Obesity and a sedentary lifestyle can contribute to the development of gynecological cancers.
Ways to Lower Gynecological Cancer Risk
- Gardasil HPV vaccine lowers the risk of cervical cancer.
- Pap Smear and HPV Test: Regular cervical screenings can detect precancerous changes and early-stage cervical cancer.
- Hormonal Contraception: Birth control pills significantly lower the risk of uterine and ovarian cancer.
Difference Between Ovarian Cysts and Ovarian Cancer
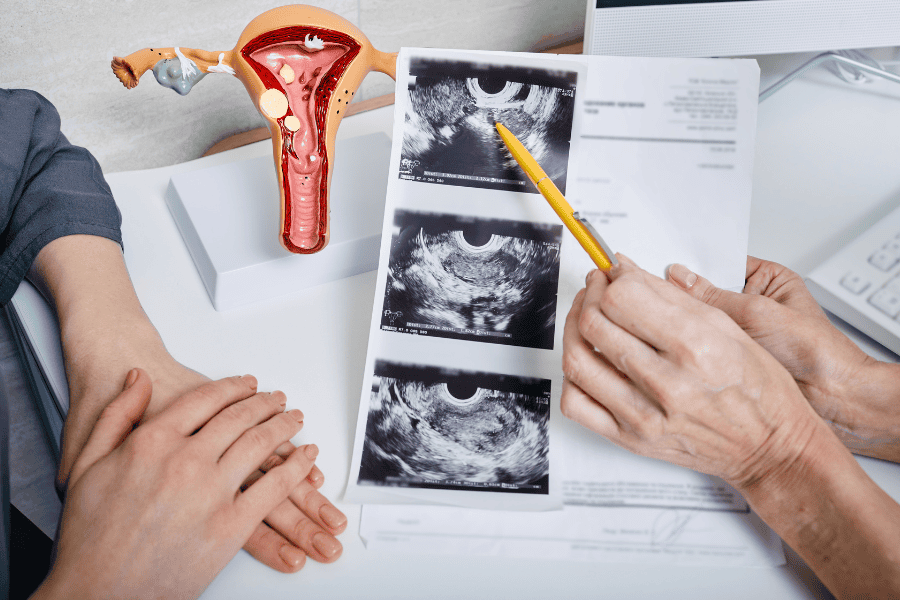 When it comes to women’s health, ovarian cysts are often confused with ovarian cancer. While both conditions affect the ovaries, they have distinct characteristics, causes, and treatments.
When it comes to women’s health, ovarian cysts are often confused with ovarian cancer. While both conditions affect the ovaries, they have distinct characteristics, causes, and treatments.
Ovarian Cysts vs. Ovarian Cancer
Although ovarian cysts and ovarian cancer develop in the same organ, they differ significantly in their nature and implications. Here’s a closer look at each condition:
Ovarian Cysts
Ovarian cysts are usually benign (noncancerous) growths that women can experience during their reproductive years. These cysts typically have a sac-like shape containing a semisolid or liquid substance. Many ovarian cysts are a byproduct of the menstrual cycle and usually resolve on their own without causing any symptoms or requiring treatment.
However, in some cases, ovarian cysts can become large or press against nearby structures, potentially causing symptoms such as:
- Pain during sex
- A frequent urge to urinate
- Lower abdominal or pelvic pain, which can occur intermittently or during menstruation
- Abdominal bloating and pressure
Although rare, ovarian cysts can rupture, causing sudden and intense pain. While certain types of ovarian cysts can become cancerous, this is uncommon.
Ovarian Cancer
Ovarian cancer is a malignant (cancerous) tumor that originates in the cells of the ovaries or fallopian tubes. It results from unusual changes (mutations) in the DNA of these cells. The exact cause of these mutations is unclear, but several factors can increase a woman’s risk of developing ovarian cancer, including:
- Being older than 50
- Having a family history of ovarian cancer
- Being overweight or obese
- Inherited gene changes, such as BRCA1 or BRCA2 mutations
- Never becoming pregnant
Unlike ovarian cysts, ovarian cancer requires prompt medical treatment. The symptoms of ovarian cancer can be similar to those of ovarian cysts and often include:
- Abdominal bloating and pressure
- A frequent urge to urinate
- Lower abdominal or pelvic pain
- Lower back pain
- Fatigue
- Changes in bowel habits, such as constipation
- Unexplained weight loss
 When to See a Doctor
When to See a Doctor
If you persistently experience any of the above symptoms, consult a gynecologist. Early diagnosis can significantly impact treatment success and outcomes. At Women First, we conduct exams and testing for all gynecological cancers. Schedule an appointment online or call 502-891-8788.
Next Steps for Gynecological Cancer Awareness
Understanding the early indicators of gynecological cancers can empower you to take charge of your health. Don’t ignore persistent symptoms or unusual changes in your body. Regular check-ups and awareness of your body’s signals significantly improve early detection and treatment.
Staying informed and proactive can help you better manage your health and well-being. Remember, it’s always better to seek medical advice from a gynecologist and rule out any serious conditions than to overlook a potential warning sign.
